Table of Content
- Health Insurance Marketplace
- Texas Medicaid will pay for a nursing home, assisted living, or home health care when a patient needs skilled nursing care.
- There is a easier way to know if you qualify for Medicaid
- Texas Medicaid Long Term Care Programs, Benefits & Eligibility Requirements
- Income Limits for Long-Term Care Through Texas Medicaid
Medicaid does not cover community-based alternatives to nursing homes by default, therefore an applicant must receive a CBA waiver if they wish to receive assistance paying for such services. As people age, they may require long-term care services to protect their health and improve their wellbeing. Nursing homes, in-home health care, and assisted living facilities are the most common long-term care services for seniors, however they’re also the most expensive. According to Genworth Financial, the average annual cost of long-term care in Texas is between $42,000 - $72,635, and for many seniors, these high costs can be a hindrance to retirement. Countable assets include cash, stocks, bonds, investments, credit union, savings, and checking accounts, and real estate in which one does not reside. There are also many assets that Medicaid considers to be exempt (non-countable).

While there are several different Medicaid eligibility groups, this page is focused on Medicaid eligibility for elderly Texas residents, aged 65 and over. In addition to nursing home care, assisted living services, and adult foster care services, Texas Medicaid pays for many non-medical support services that help frail seniors remain living in their homes. STAR+PLUS members receive their benefits through a single Medicaid plan provided by a managed care organization , which has a network of healthcare providers. This means the beneficiary can choose a caregiver from outside the MCO network, including some family members.
Health Insurance Marketplace
In most cases, the doctor’s opinion that the applicant should be living in an assisted living or nursing facility is sufficient. PACE is intended to help Texas residents who need a Nursing Facility Level of Care but want to keep residing and receiving care in their home or somewhere else in the community. This program can be used by people who are “dual eligible” for Medicaid and Medicare and will help them coordinate the care from those two programs. Many Texas residents will receive their long term care Medicaid benefits through the STAR+PLUS Program, which is also known as the STAR+PLUS Waiver, and the STAR+PLUS Home and Community-Bases suite of services.
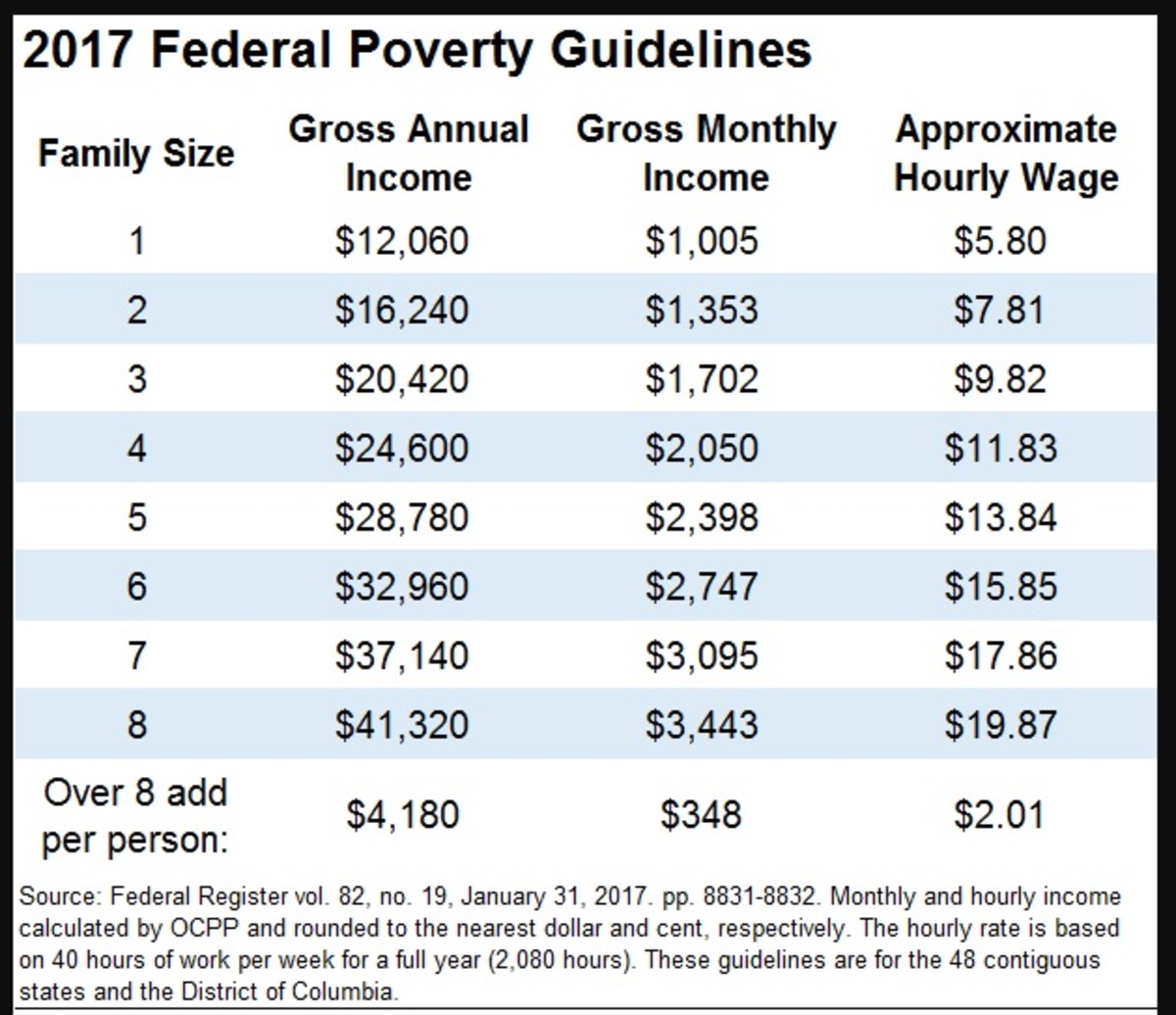
Texas residents have to meet an asset limit and an income limit and in order to be financially eligible for Home and Community Based Service Waivers. A Miller Trust allows seniors to transfer some of their income to an “income trust” without facing a penalty from Medicaid. Income trusts are exempt from Medicaid consideration, as their primary purpose is to pay for a person’s care costs. When an applicant transfers all of their resources which exceed Medicaid’s limits into a Miller Trust, they can effectively reduce their income and improve their eligibility for benefits. For example, if a person earns $3,250 a month in non-exempt income, they will theoretically disqualify themselves from Medicaid.
Texas Medicaid will pay for a nursing home, assisted living, or home health care when a patient needs skilled nursing care.
To be eligible for Texas Medicaid, a person has to meet certain financial requirements and functional requirements. Any Texas Medicaid beneficiary who receives Nursing Home Medicaid coverage must give most of their income to the state to help pay for the cost of the nursing home. This can be spent on any personal item – clothes, snacks, books, haircuts, cell phones, etc. In order for an applicant to create nursing home medicaid eligibility in terms of resources, they must not have more than $2,000 in counted resources. It is possible for an applicant to qualify for Medicaid if they own more than $2,000 in assets, as some property is exempt from consideration.
Various long-term care benefits, such as personal care assistance or adult day care, may be available. Medicaid will cover the cost of long term care in a nursing home for eligible Texas residents through its Nursing Home / Institutional Medicaid. This includes payment for room and board, as well as all necessary medical and non-medical goods and services. These can include skilled nursing care, physician’s visits, prescription medication, medication management, mental health counseling, social activities and assistance with Activities of Daily Living .
There is a easier way to know if you qualify for Medicaid
Most Medicaid beneficiaries in Texas receive services through a managed care system. Managed care systems allow Medicaid beneficiaries to choose a qualified plan from a pre-approved list of providers serving their location, and choose a physician who is covered by their chosen plan. Private insurance providers create a contract with the state of Texas to offer Medicaid services, allowing managed care systems to work. The primary managed care system most people use is known as the State of Texas Access Reform Managed Care program. 1) STAR+PLUS Waiver – This is a limited enrollment, managed care program that covers assisted living, adult foster care, and many in-home supports to help beneficiaries avoid nursing home placement.

By working with a Medicaid planning professional, families can employ a variety of strategies to help them become Medicaid eligible, as well as to protect their home from Medicaid’s estate recovery program. All assets of a married couple are considered jointly owned regardless of the long-term care Medicaid program for which one is applying. However, the non-applicant spouse of an Institutional Medicaid or Medicaid Waiver applicant is permitted a Community Spouse Resource Allowance . In 2022, the community spouse (the non-applicant spouse) can retain 50% of the couples’ assets, up to a maximum of $137,400, as the chart indicates above. If the non-applicant’s half of the assets is under $27,480, 100% of the assets, up to $27,480 can be retained by the that spouse. 3) Regular Medicaid / Elderly and People with Disabilities – This is an entitlement program; Persons who meet the eligibility requirements are guaranteed program benefits.
Each applicant is allowed one burial fund exclusion, provided it is worth $1,500 or less. Additional vehicles will qualify as non-exempt assets, and will count toward the applicant’s asset limit. Resources are assets, like money in the bank, retirement accounts, land, and personal property like cars.
A caregiver agreement is one way seniors transfer assets without incurring penalties from Medicaid. When two people enter into a caregiver agreement, one party is paying the other to help them with a task For example, a person’s mother may pay them to do laundry, which would ordinarily count as a voluntary funds transfer. If the two individuals have a caregiver agreement, and the amount being paid is reasonable for the assistance being provided, Medicaid will not assign a penalty for the funds transfer. Burial accounts, funeral trusts, and end-of-life expense accounts may also qualify as exempt assets if they meet Medicaid’s criteria.
For 2018 there were small increases in the substantial home equity limit, the minimum Community Spousal Protected Amount, and the maximum Community Spousal Protected Amount. During open enrollment, you can apply for cost assistance, change plans, and enroll in a plan. If you need help qualifying for Medicaid, a skilled Medicaid planning attorney can also help you with asset protection planning. After an applicant has been approved for Nursing Home Medicaid through Texas Medicaid, they need to choose which Medicaid-approved nursing home they will live in.
By qualifying as an “entitlement” program, PHC is accessible to anyone who meets the eligibility requirements. Assisted living facilities provide food, personal care services like help with bathing or dressing, and medication administration. However, Texas has a program offering Medicaid payment for assisted living facilities, if you meet specific criteria.
When chronic conditions make it challenging or impossible for seniors to complete their ADLs independently, long-term care services can qualify as medical necessities. For a person to qualify for the PHC Program, they must be eligible for Medicaid. They must require assistance with at least one daily activity , and a medical condition, as documented by a licensed physician, must be the reason they need assistance. There are no additional financial qualifications a person must meet to qualify for the PHC Program - if a person meets Medicaid’s asset and income limits, they may financially qualify for PHC. Seniors in Texas who need in-home personal assistance to complete their activities of daily life may qualify for coverage through the Primary Home Care Program. The PHC is an entitlement program for seniors in Texas who require assistance with essential daily tasks, like changing clothes, showering, eating, and attending to calls of nature.

No comments:
Post a Comment