Table of Content
Prior to applying for Medicaid benefits in Texas, it is imperative that seniors be certain that all eligibility requirements for the program in which they are applying are met. Persons who have income and / or assets over the limit, or are unsure if they meet the eligibility criteria, should seriously consider Medicaid planning. For additional information about applying for long-term care Medicaid, click here. When only one spouse of a married couple applies for Institutional Medicaid or a Medicaid Waiver, only the income of the applicant is counted.

Medicaid does not cover community-based care by default, however there are numerous programs in Texas which may extend a person’s benefits to include alternative forms of care. Medicaid can help with this often overwhelming endeavor — but you might not know where to begin. However, if you know that you will need care in the immediate or distant future, you can save yourself stress and worry by planning for Medicaid now. The first step is for you to find out if you meet the Texas state Medicaid eligibility requirements. Many seniors attempt to qualify for Medicaid by transferring some of their resources to friends and family members prior to applying for benefits. Medicaid defines these voluntary transfers as gifts, and they can have a major impact on a person’s eligibility to receive benefits.
Nursing Home Medicaid Income and Asset Rules
By working with a Medicaid planning professional, families can employ a variety of strategies to help them become Medicaid eligible, as well as to protect their home from Medicaid’s estate recovery program. All assets of a married couple are considered jointly owned regardless of the long-term care Medicaid program for which one is applying. However, the non-applicant spouse of an Institutional Medicaid or Medicaid Waiver applicant is permitted a Community Spouse Resource Allowance . In 2022, the community spouse (the non-applicant spouse) can retain 50% of the couples’ assets, up to a maximum of $137,400, as the chart indicates above. If the non-applicant’s half of the assets is under $27,480, 100% of the assets, up to $27,480 can be retained by the that spouse. 3) Regular Medicaid / Elderly and People with Disabilities – This is an entitlement program; Persons who meet the eligibility requirements are guaranteed program benefits.

This article focuses on Texas Medicaid Long Term Care, which is different from regular Medicaid. In order for an applicant to create nursing home Medicaid eligibility with their income, they must not receive more than $2,523 in income each month. A small percentage of seniors have private long-term care insurance policies to pay for their long-term care. To incentivize more seniors to purchase long-term care insurance and thus prepare for their future, Texas Medicaid operates in coordination with the nation’s Long-Term Care Partnership Program .
Health Requirements
For example, if a person’s long-term care policy pays $50,000 toward their care, Medicaid may allow them to retain $50,000 in countable assets. Seniors who do not financially qualify for Medicaid may become eligible using exemptions through the Long-Term Care Partnership Program. Medicaid applicants with retirement accounts (like IRAs or 401s) may have to count them toward their asset limits, depending on the account’s availability for withdrawal. All retirement accounts which are available to withdraw are non-exempt assets, and Medicaid can use them to disqualify a person from receiving benefits. Alternatively, any retirement accounts which are not available for withdrawal are exempt. If the account owner can only receive their funds through terminating their employment, a loan, or another “approved hardship,” the account may qualify as exempt.
The HHSC works jointly with the federal government to fund Texas Medicaid, with the federal government funding 57.5 percent of the program. Texas state government pays for the remaining 42.5 percent of their Medicaid spending. Our detailed book, Thinking Beyond Tomorrow, answers questions about Medicaid and paying for Long Term Care.It reviews the law, provides understandable insights, and gives strategies to help qualify for Medicaid benefits. In Texas, the home you live in is excluded from the resource calculation as long as it is worth less than $585,000 . Learn how to get nursing home care for a parent or spouse without going broke. Benefits of both the CFC and PHC programs include help with Activities of Daily Living – mobility, bathing, dressing, eating and toileting – as well as housekeeping, shopping and transportation.
When Medicaid in Texas Will Pay for a Nursing Home, Assisted Living, or Home Health Care
While there are several different Medicaid eligibility groups, this page is focused on Medicaid eligibility for elderly Texas residents, aged 65 and over. In addition to nursing home care, assisted living services, and adult foster care services, Texas Medicaid pays for many non-medical support services that help frail seniors remain living in their homes. STAR+PLUS members receive their benefits through a single Medicaid plan provided by a managed care organization , which has a network of healthcare providers. This means the beneficiary can choose a caregiver from outside the MCO network, including some family members.
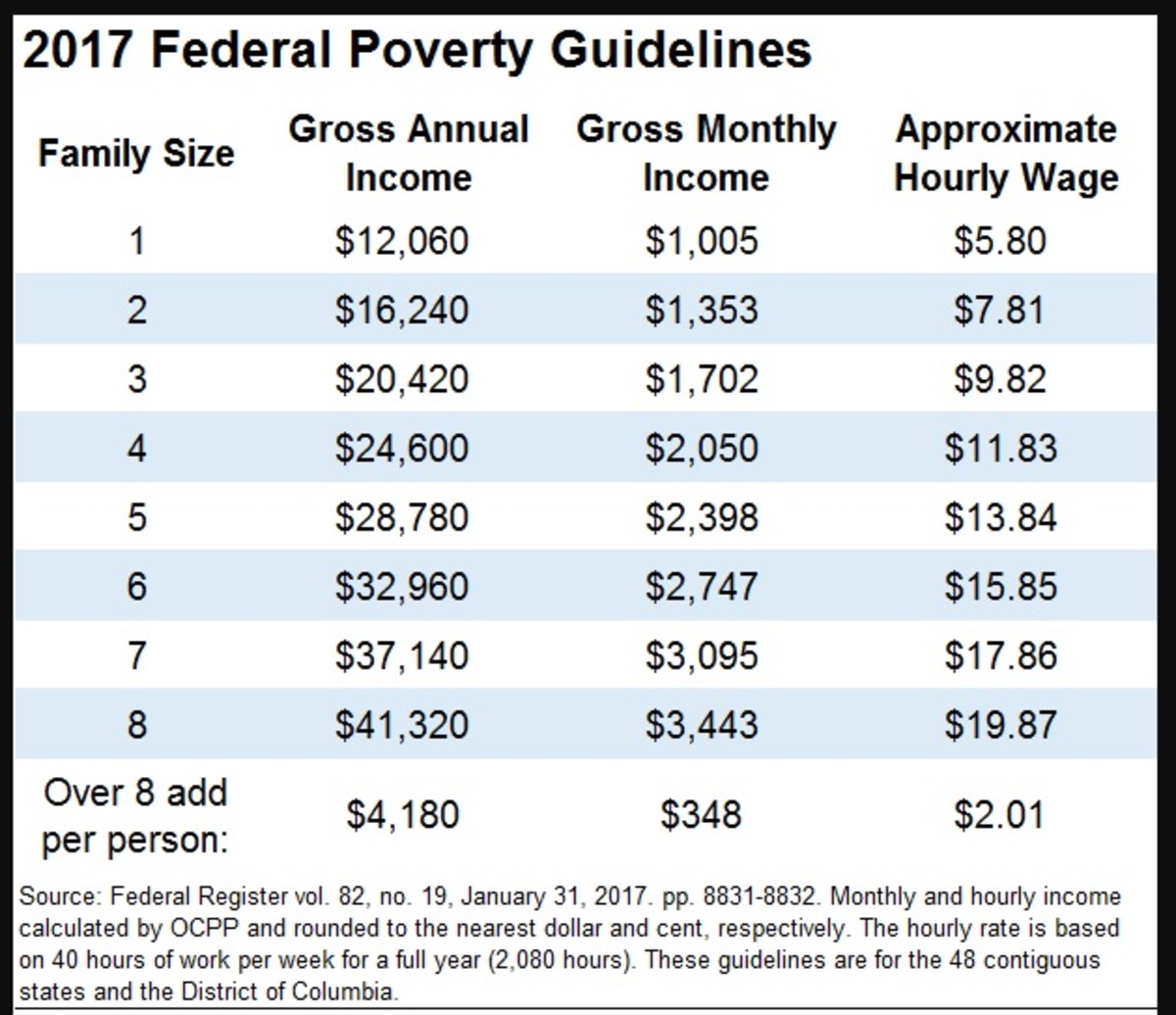
If your loved one is over that eligibility limit you can still create Medicaid eligibility with a 100% guaranteed Miller Trustfrom The Shea Law Firm. If your loved one is over the income limit and they do not have a properly created and administered Miller Trust then you are facing ineligibility for Medicaid benefits. To see if you qualify for these programs, you can go through Healthcare.gov’s page andsee if your income falls in the range to save. Categorical requirements – A person can only become eligible for Medicaid if they are at least 65 years old, blind, pregnant, or otherwise disabled. Undocumented aliens might be eligible for Medicaid only for emergency coverage. For older adults and persons with physical or intellectual disabilities, long-term care can become expensive.
Medicaid & CHIP
By qualifying as an “entitlement” program, PHC is accessible to anyone who meets the eligibility requirements. Assisted living facilities provide food, personal care services like help with bathing or dressing, and medication administration. However, Texas has a program offering Medicaid payment for assisted living facilities, if you meet specific criteria.

In 2018, the average monthly cost of a private room in a nursing home in Texas was approximately $6,540, or over $78,000 per year. Nursing homes are residential facilities that offer 24-hour skilled nursing care in addition to other supportive services. The second change is an increase in the Medicaid Applicant's gross monthly income limit.
Texas has a 5-year Medicaid Look-Back Period that immediately precedes one’s Medicaid application date. If a Medicaid applicant has gifted assets or sold them under fair market value, a period of Medicaid ineligibility will be determined. This is because it is assumed assets were transferred to meet Medicaid’s asset limit.

Irrevocable means that the terms of the trust cannot be altered or canceled. In a nutshell, a Medicaid applicant’s “excess” income is deposited into the QIT and is no longer counted towards Medicaid eligibility. A designated trustee manages the trust and can only use funds for designated purposes, such as paying unreimbursed medical expenses of the Medicaid enrollee.
While one’s home is usually exempt from Medicaid’s asset limit, it is not exempt from Medicaid’s estate recovery program. Following a long-term care Medicaid beneficiary’s death, the Medicaid agency in Texas attempts reimbursement of care costs through whatever estate of the deceased still remains. Without proper planning strategies in place, the home will be used to reimburse Medicaid for providing care rather than going to family as inheritance. One’s home is often their most valuable asset, and if counted towards Texas Medicaid’s asset limit, it would likely cause them to be over the limit for eligibility. However, in some situations the home is not counted against the asset limit.
You do not need to meet the nursing home level of care to qualify for home health services. However, because these Medicaid-funded home health services are related to a doctor's plan of care for a particular medical condition, they are generally offered on a short-term basis. Texas also offers continuing care retirement communities , which combine independent living, assisted living, and nursing home care in one residential setting. CCRCs, which are regulated by the Texas Department of Insurance, typically charge entrance and monthly fees. Once in a CCRC, you can use long-term care insurance, private insurance, Medicare, or Medicaid to pay for some of your health care, depending on your coverage options and the types of services you require. STAR+PLUS is Texas' Medicaid managed care program for people who have disabilities or who are 65 and over.
Eligibility is generally based on income and family status, but some states have different rules. The second step is determining if the applicant meets the financial and functional criteria, also discussed above, for that Long Term Care program. Applying for Texas Medicaid when not financially eligible will result in the application, and benefits, being denied.